Unlocking Early Detection: The Role of Skin Biomarkers in ALS
Amyotrophic lateral sclerosis (ALS) is a devastating neurodegenerative disease that leads to the progressive loss of motor neurons in the brain and spinal cord, ultimately resulting in muscle weakness and paralysis. The prognosis is grim, with the majority of patients succumbing to the disease within three to five years of symptom onset. While existing treatments like riluzole can modestly slow disease progression, they do not stop it altogether. The need for early diagnosis has never been more pressing, given that early intervention can significantly improve patient outcomes.
Current Diagnostic Challenges and the Need for Innovation
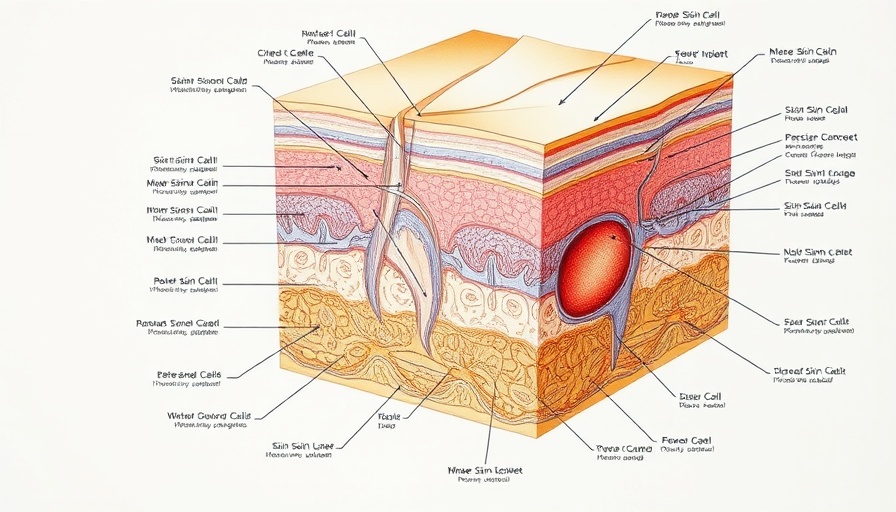
Diagnosing ALS presents numerous challenges; common methods like neurological exams, electromyography, and imaging often lead to inconclusive results, causing critical delays of over a year in many cases. Blood tests have not proven reliable due to their lack of specificity, and invasive procedures like cerebrospinal fluid sampling are not routinely practical. As a result, researchers are exploring the skin as a promising diagnostic tool for ALS. The skin, sharing an embryonic origin with the central nervous system, may reflect the cellular and molecular changes that occur within the nervous system.
Insights from Skin Biomarkers
Recent studies have unearthed intriguing correlations between ALS and skin abnormalities. For instance, disorganized collagen fibers and thickened blood vessel walls have been detected, as well as vascular changes characterized by "onion-skin" formations. Importantly, reduced density of sensory and autonomic nerve fibers in the skin could signal earlier symptoms of the disease well before neurological deficits manifest.
Moreover, the presence of specific proteins associated with ALS, such as SOD1, TDP-43, and FUS, have been observed in skin fibroblasts. This indicates that the pathological changes seen in ALS may extend beyond the central nervous system, underscoring the systemic nature of the disease.
Future Aspirations: Bridging Research with Clinical Practice
The idea of using skin-based biomarkers as a diagnostic tool for ALS opens the door to a more accessible and non-invasive means of early detection. If proven effective, this method could revolutionize the way we approach ALS diagnosis, offering patients a better chance for early intervention. Ongoing research is essential to validate these findings and to determine standardized protocols for integrating skin biopsies or assessments into regular clinical practice.
The Broader Implications: What This Means for Patients and Families
An earlier diagnosis could empower patients and their families to make informed decisions regarding their treatment options, lifestyle changes, and palliative care. Beyond the direct medical implications, this advancement resonates emotionally; families may experience less uncertainty during the challenging journey of an ALS diagnosis. By improving the likelihood of early detection, the sadness and confusion that often accompany the journey can potentially be mitigated.
Concluding Thoughts: A Call for Continued Research
The exploration of skin-based biomarkers in ALS research presents an exciting frontier with significant promise. As science delves deeper into the connection between skin health and neurodegenerative diseases, it emphasizes the need for innovative approaches to diagnosis and treatment. Future research could yield groundbreaking methods that not only facilitate quicker diagnosis but also enhance our understanding of ALS pathology.
As professionals and advocates in the field, it is paramount to support ongoing research efforts aimed at further understanding this complex disease. Working collaboratively within the medical and scientific communities, we can strive to bring forth advancements that make a meaningful impact on patients' lives.
 Add Row
Add Row  Add
Add 




Write A Comment