
Revolutionizing Type 1 Diabetes Treatment with 3D-Printed Islets
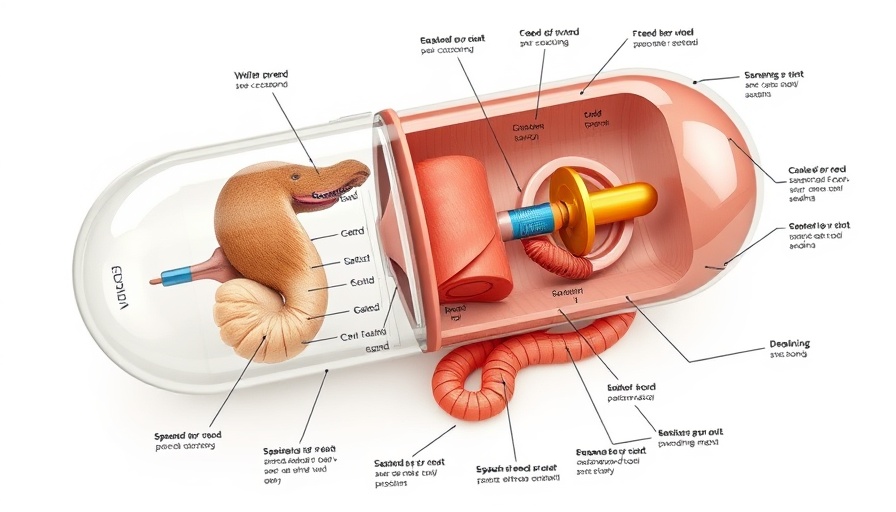
A groundbreaking advancement in diabetes research was presented at the 2025 ESOT Congress. Scientists have successfully 3D-printed functional human islets, which could change the treatment landscape for type 1 diabetes (T1D). This method employs a novel bioink, combining alginate with decellularized human pancreatic tissue, to create islet structures that not only survive but remain functional for an extended period.
What Makes This Breakthrough Unique?
Traditionally, islet transplants involve a significant risk of cell loss, especially when infused into the liver. The innovative 3D printing approach allows for implantation just under the skin, requiring only local anesthesia. This less invasive method holds promise for improved patient comfort and outcomes.
How They Did It: The Science Behind the Technology
The lead researcher, Dr. Quentin Perrier, emphasized the importance of mimicking the pancreas's natural environment through careful bioink selection. By using a special bioink that replicates the supportive structure found in the pancreas, the islets are provided with necessary nutrients and oxygen. Key parameters, such as low pressure and slow print speed, were fine-tuned to ensure the delicate islets maintained their integrity throughout the printing process.
The Promising Results of Laboratory Tests
Early tests demonstrated that the bioprinted islets achieved over 90% cell survival and had enhanced responses to glucose. By day 21, these islets exhibited a remarkable ability to sense blood sugar levels, crucial for effective diabetes management. Unlike conventional preparations, the printed structures maintained their shape and functionality, presenting a significant shift in treatment potential.
Future Implications and Benefits for Diabetes Treatment
This new printing technology could spell a new era in managing T1D, providing patients with access to a treatment that is both safer and more effective than traditional methods. The porous architecture of the islets improves oxygen and nutrient flow, further augmenting their viability post-transplant.
Overcoming Challenges in Bioprinting
This development also addresses prior hurdles experienced in bioprinting, such as clumping and structural degradation. By creating a stable and supportive environment for islets, scientists are one step closer to making functional islet therapy a reality for diabetic patients.
The path forward looks promising. As this technology advances, the goal is to achieve a solution not only for type 1 diabetes but possibly other conditions requiring tissue regeneration, setting the stage for more extensive applications in regenerative medicine.
 Add Row
Add Row  Add
Add 



 Add Row
Add Row  Add
Add 
Write A Comment